Shoulder Instability - Traumatic >> Treatment
How is a dislocation and traumatic shoulder instability treated?The initial reduction of a dislocation can be quite difficult. Contractions of the shoulder muscles can trap the humeral head against the glenoid. Gentle traction, and at times, medication may be needed to accomplish the reduction. Once the shoulder is reduced, a sling is used for a few days to protect it, and relieve discomfort. Physical therapy may help the patient regain motion in the joint.
Non-Operative Treatment
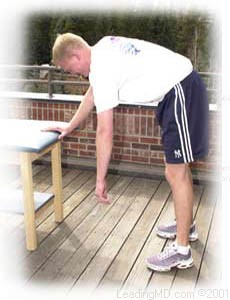
Initial treatment for recurrent instability of the shoulder centers on physical therapy. Strengthening the rotator cuff muscles and periscapular muscles (those around the scapula) gives stability to the joint. The goal of physical therapy is to help the muscles provide stability to the shoulder that the torn ligaments can no longer supply. The therapy for recurrent instability should be carefully designed for each patient since this condition often causes apprehension about certain arm positions or exercise maneuvers. Very often, physical therapy can help regain lost motion, reduce apprehension, and restore shoulder function.
Operative Treatment
Surgery is usually recommended if recurrent instability cannot be controlled with physical therapy and activity modification. The goal of surgery is to return stability to the shoulder with the least loss of motion. All shoulder procedures designed to stabilize the shoulder involve some loss of motion. The current procedures for anterior shoulder instability attempt to restore the normal anatomy without over tightening the ligaments. In certain instances, such as in young persons who have a higher risk of re-dislocation and in contact athletes who plan on continuing to participate in sports that put their shoulders at risk, surgery may be performed after the first dislocation.
 |
|
Use the bottons above to see the different steps. |
Open Labral Repair
Currently, the preferred procedure for anterior instability is an open labral repair with an anterior capsular shift. This procedure is performed through a two to three inch incision on the front of the shoulder. The torn labrum is repaired and the stretched-out anterior shoulder capsule is imbricated (overlapped) to make it smaller. This procedure is successful approximately 95% of the time in eliminating recurrent dislocations.
Arthroscopic Techniques
Recently, arthroscopic procedures such as Bankart repair have been used to repair the torn labrum and reduce capsular laxity. Arthroscopic techniques are approximately 80% successful. These procedures are performed with visualization through a small fiberoptic scope. Instruments are inserted into the joint through two or three small incisions to repair the labrum. The surgical technique is similar to the one used in an open repair. A loose capsule is more difficult to address arthroscopically. Procedures using thermal energy to shrink the loose capsule have been developed, and are still being evaluated.
What types of complications may occur?
The major complications of anterior stabilization techniques are recurrent instability and/or loss of motion. The rate of recurrent instability depends largely on the technique used for the repair. The loss of motion can be severe, and is a function of over tightening the anterior capsule. In general, the operative shoulder should lose no more than ten degrees of external rotation. Other small risks (less than 1%) include infection, post-operative stiffness, nerve damage, or blood vessel injury.